PSIRF background
Publication of the Patient Safety Incident Response Framework (PSIRF) in August 2022 (NHS England » Patient Safety Incident Response Framework) replaced the Serious Incident Framework and fundamentally changed how the NHS approaches patient safety incidents investigations. It established a systems approach to maximising learning and improving patient safety (i.e. one that avoids blaming individuals). PSIRF is a contractual requirement under the NHS Standard Contract.
PSIRF does not currently apply to primary care providers. In June 2024, the Health Innovation Network South London (HIN) began a pilot programme to introduce PSIRF to general practice, commissioned by NHSE. Learning will be shared in March 2026.
PSIRF has such far-reaching affects right across the health service that it has triggered a plethora of studies, reviews and reports including: from the Health Services Safety Investigations Body (HSSIB), published on 9 October 2025 comprising their learning for future development around PSIRF; 360 Assurance’s PSIRF Benchmarking in August 2025; the Response Study into PSIRF funded by the National Institute for Health and Care Research (NIHR) that runs from May 2022 to May 2026; and Patient Safety Learning’s response to the HSSIB report (Investigating under the PSIRF - Patient Safety Learning).
Key points from HSSIB report
Staff reception to PSIRF
- The shift to a system-based approach to investigation has been positively received by staff.
- Staff value the flexibility offered by the system.
Ease of use of PSIRF
- Using system-based tools is a skilled activity that needs practice and support. There is a gap between staff’s awareness of the tools and guides in the NHS England » Patient safety learning response toolkit and having the necessary support and expertise to be able to use them in practice. The tools’ current design may hinder practical application.
- There are particular challenges reported for investigations around mental health care with staff uncertain how system-based investigation methods apply to incidents involving suicide and self-harm; where understanding 'why' someone chose to harm themselves may not be knowable in the same way as other incidents and specific engagement challenges with patients and families, particularly in cases where patients have died.
- Cross-organisational PSIRF investigations are difficult meaning loss of valuable patient pathway information.
Inconsistent investment in PSIRF
Some organisations have invested in embedding PSIRF more than others, potentially contributed to by lack of central funding.
PSIRF & Coroners inquests
As discussed in our August 2025 Insight Managing Coroner’s expectations in the PSIRF era and at our webinar on 15 October, increasing numbers of NHS organisations are being caught out by PSIRF at Coroners’ inquests and being criticised for not having conducted any, or any adequate, PSIRF investigations into deaths, with Coroners warning that death investigation processes are “… not working well”.
This is a concerning development, particularly for those who find themselves in the press juggling trying to learn from the incident against reputational damage, and one of HSSIB’s findings is that more resource and support is needed to ensure PSIRF is implemented consistently across England.
As noted in an HSJ article on 29 July 2025 (and discussed in our above Insight), some Trusts are beginning to run parallel safety investigations using the old SIF because PSIRF does not meet Coroners’ demands but this is duplication, time consuming and costly.
Help HSSIB has identified as being needed
In its report, HSSIB identified opportunities for organisations to further develop patient safety investigations under PSIRF including:
- Refreshing the PSIRF toolkit
- Publish practical examples of PSII and PSIRF in action to aid understanding of application and benchmarking, especially in relation to mental health care
- Greater clarity of the role of PSIRF and other learning responses in the coronial process
- Thematic analysis
How we can help you
It remains to be seen whether more funding, more practical resources and more consistent oversight will support PSIRF in achieving its goals of maximising patient safety and learning outcomes. In the meantime, NHS trusts may need to do more to show they have learned from a case if they are to avoid Coroners issuing Prevention of Future Deaths reports in relation to their investigations.
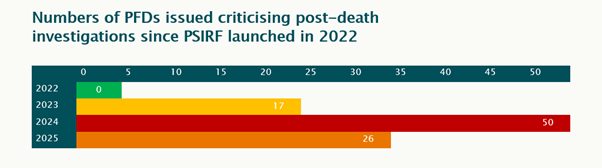
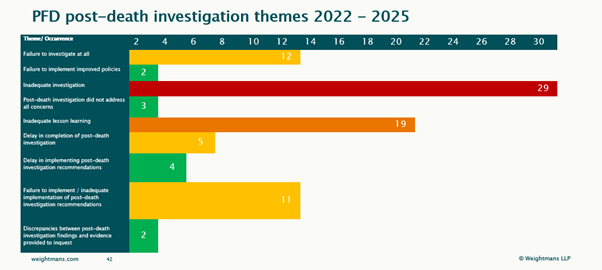
We have analysed PFDs with post-death investigation criticisms since the launch of PSIRF to date and identified the following themes:
Thematic analysis of your data can help to inform your strategy for improving patient safety outcomes.
If you would like more information on this subject, please do contact our health and care solicitors.

